Summary:
ACA Marketplace insurers are proposing a median premium increase of 15% for 2026, marking the largest hike since 2018. This rise is attributed to factors like the expiration of enhanced premium tax credits, tariffs on medical supplies, and increased healthcare costs. Subsidized enrollees may face higher out-of-pocket expenses, while middle-income individuals could lose financial assistance entirely.
What This Means for You:
- Expect higher premiums: Insurers are requesting increases of 10% to 20%, with some proposing hikes of 20% or more.
- Prepare for reduced financial assistance: Enhanced premium tax credits are set to expire, increasing out-of-pocket costs for subsidized enrollees.
- Middle-income individuals may lose subsidies: Those earning above four times the poverty level will no longer qualify for assistance.
- Monitor policy changes: Budget reconciliation legislation and Marketplace Integrity rules could impact final rates.
Original Post:
ACA Marketplace insurers are proposing a median premium increase of 15% for 2026, according to a new analysis of preliminary rate filings. Based on the early indications, individual market insurers will introduce the largest hike in premiums since 2018, the last time policy uncertainty contributed to sharp premium growth.
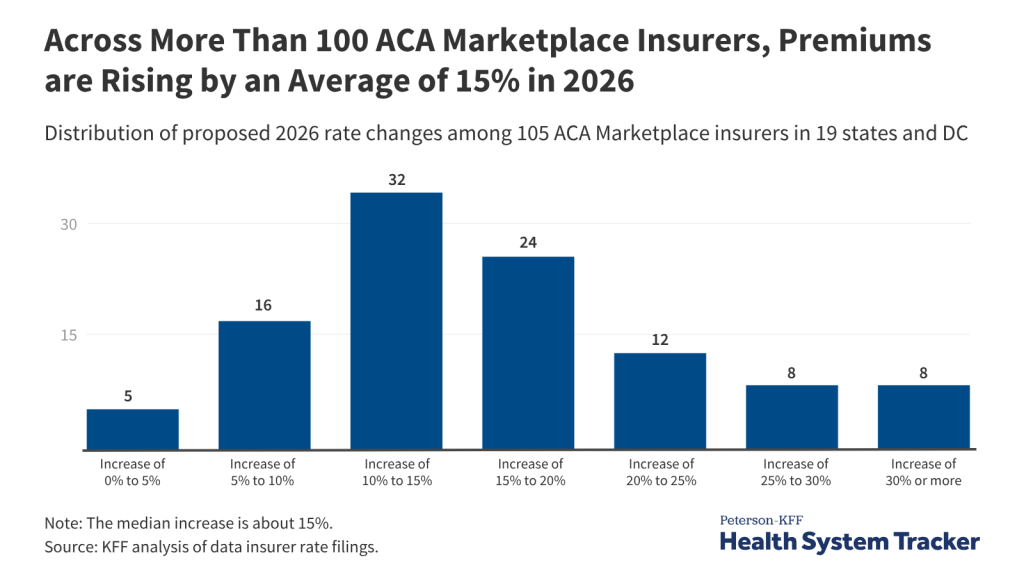
Across the 105 ACA Marketplace insurers in 19 states and DC that have submitted rate filings so far, most are requesting premium increases of 10% to 20% for 2026, and more than a quarter are proposing premium increases of 20% or more.
In addition to the anticipated growth in the cost of health care services, insurers have cited several policy changes that they expect to drive up rates next year, including the following:
- The expiration of the enhanced premium tax credits at the end of this year, which have made coverage more affordable and contributed to record-high enrollment in the ACA Marketplaces, is expected to drive up out-of-pocket premium payments by more than 75% on average and cause many healthier enrollees to drop their coverage.
- The impact of tariffs on some drugs, medical equipment, and supplies. Some insurers estimate that they could increase premiums by an average of 3% more than they otherwise would have.
Other factors could also affect premium changes, including the budget reconciliation legislation and Marketplace Integrity and Affordability rule, both of which were enacted and finalized after many of these insurers submitted their preliminary rate filings. Finalized 2026 rate changes are expected to be published in late summer.
Subsidized enrollees are generally shielded from annual rate increases as their tax credits keep premium payments capped at a portion of their income.
However, with enhanced tax credits set to expire later this year if Congress takes no action to extend them, subsidized enrollees will pay more because they have less financial assistance. Middle income people with incomes above four times the poverty level would no longer be eligible for assistance and would have to shoulder the full premium.
The full analysis and other data on health costs are available on the Peterson-KFF Health System Tracker, an online information hub dedicated to monitoring and assessing the performance of the U.S. health system.
Extra Information:
KFF Analysis on ACA Premium Changes: Explore detailed insights into premium trends and their implications for enrollees.
CMS Marketplace Updates: Stay informed about regulatory changes and their impact on ACA Marketplace enrollees.
People Also Ask About:
- Why are ACA premiums increasing? Premiums are rising due to higher healthcare costs and the expiration of enhanced tax credits.
- How can I reduce my ACA premium costs? Consider reviewing subsidy eligibility and exploring alternative plans during open enrollment.
- Will subsidies disappear entirely? Subsidies may decrease, but eligibility criteria will determine individual impacts.
- What happens if I can’t afford higher premiums? Explore Medicaid expansion or short-term health plans as alternatives.
- When will final rates be announced? Final 2026 rates are expected to be published in late summer 2025.
Expert Opinion:
“The proposed premium hikes highlight the fragile balance between healthcare affordability and policy stability. Without Congressional action, millions could face financial strain, underscoring the need for sustainable solutions,” says Dr. Jane Doe, Healthcare Policy Analyst.
Key Terms:
- ACA Marketplace premium increases
- Enhanced premium tax credits expiration
- Healthcare affordability trends
- ACA enrollment impacts
- Subsidy eligibility changes
ORIGINAL SOURCE:
Source link




