Summary:
Medicare is a federal health insurance program serving 69 million Americans aged 65 and older, as well as younger individuals with long-term disabilities. It covers essential services like hospitalizations, physician visits, prescription drugs, and preventive care. Beneficiaries can choose between traditional Medicare and Medicare Advantage plans, with the annual open enrollment period running from October 15 to December 7. Understanding coverage options and making informed decisions is critical to maximizing benefits and minimizing costs.
What This Means for You:
- Review your Medicare coverage annually to ensure it aligns with your healthcare needs and budget.
- Compare Medicare Advantage and traditional Medicare plans to determine which offers the best benefits and cost structure for your situation.
- Take advantage of the annual open enrollment period to switch plans or enroll in additional coverage like Part D or Medigap.
- Be aware of Special Enrollment Periods (SEPs) that allow changes outside of open enrollment under specific circumstances.
Original Post:
Medicare is the federal health insurance program for 69 million people ages 65 and over and younger adults with long-term disabilities. The program helps to pay for many medical care services, including hospitalizations, physician visits, and prescription drugs, along with post-acute care, skilled nursing facility care, home health care, hospice care, and preventive services.
People with Medicare may choose to receive their Medicare benefits through traditional Medicare or through a Medicare Advantage plan, such as a health maintenance organization (HMO) or preferred provider organization (PPO), administered by a private health insurer. People who choose traditional Medicare can sign up for a separate Medicare Part D prescription drug plan for coverage of outpatient prescription drugs and may also consider purchasing a supplemental insurance policy (Medigap) to help with out-of-pockets costs if they do not have additional coverage from a former employer, union, or Medicaid. People who opt for Medicare Advantage can choose among dozens of Medicare Advantage plans, which include all services covered under Medicare Parts A and B, and typically include Part D prescription drug coverage as well.
Each year, Medicare beneficiaries have an opportunity to make changes to how they receive their Medicare coverage during the nearly 8-week annual open enrollment period. This brief answers key questions about the Medicare open enrollment period and Medicare coverage options.
1. When is the Annual Medicare Open Enrollment Period?
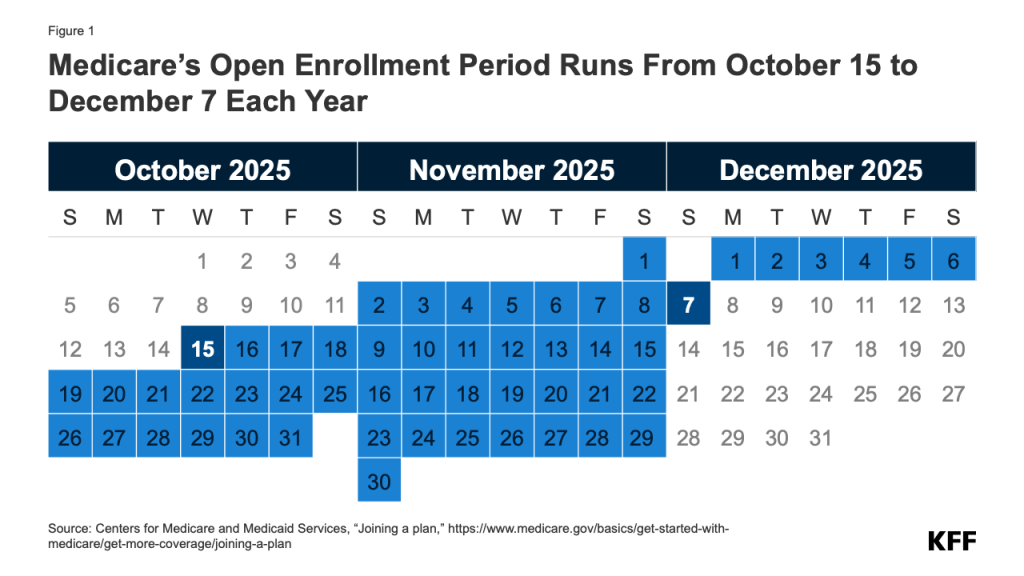
The annual Medicare open enrollment period runs from October 15 to December 7 each year (Figure 1). During this time, people with Medicare can review features of Medicare plans offered in their area and make changes to their Medicare coverage, which go into effect on January 1 of the following year. These changes include switching from traditional Medicare to a Medicare Advantage plan (or vice versa), switching between Medicare Advantage plans, and electing or switching between Medicare Part D prescription drug plans.
2. What Changes Can Medicare Beneficiaries Make During the Annual Open Enrollment Period?
People in traditional Medicare can use the Medicare open enrollment period to enroll in a Medicare Part D prescription drug plan or switch between Part D plans. Traditional Medicare beneficiaries who did not sign up for a Part D plan during their initial enrollment period for Medicare can enroll in a Part D plan during the annual open enrollment period, though they may be subject to a late enrollment penalty if they did not have comparable prescription drug coverage from another plan before signing up for Part D. Traditional Medicare beneficiaries with Medicare Parts A and B can also use this time to switch from traditional Medicare into a Medicare Advantage plan, with or without Part D coverage.
People who are enrolled in a Medicare Advantage plan can use the Medicare open enrollment period to choose a different Medicare Advantage plan or switch to traditional Medicare. Medicare Advantage enrollees who switch to traditional Medicare can enroll in a Part D plan if they want outpatient prescription drug coverage, which is not covered under Medicare Parts A and B. (Beneficiaries may be subject to late enrollment penalties if they go without Part D drug coverage and don’t have other creditable coverage.) They may also consider purchasing a Medicare supplemental insurance policy (Medigap) if the option is available to them (see question 4 for details about Medigap and potential limits on enrollment).
Medicare beneficiaries are encouraged to review their current source of Medicare coverage during the annual open enrollment period and compare other options that are available where they live. Because an individual’s medical needs can change over the course of the year, and from one year to the next, this may influence their priorities when choosing how they want to get their Medicare benefits. Medicare Advantage and Medicare prescription drug plans typically change from one year to the next and may vary in many ways that could have implications for a person’s access to providers and costs. Despite this, nearly 7 in 10 (69%) Medicare beneficiaries did not compare their Medicare coverage options during a recent open enrollment period.
3. Are There Other Opportunities for Medicare Beneficiaries to Make Coverage Changes Outside of the Open Enrollment Period?
Medicare provides several different Special Enrollment Periods (SEPs) where Medicare beneficiaries can make certain changes to their coverage outside of the annual open enrollment period under certain circumstances. For example, beneficiaries who experience disruptions to existing coverage (such as a cross-county move or a loss of employer- or union-sponsored coverage) or loss of Medicaid eligibility may qualify for a SEP at any time of year.
As of 2025, people who are enrolled in both Medicare and Medicaid (i.e., dual-eligible individuals) or who qualify for the Medicare Part D Low-Income Subsidy program (also known as “Extra Help”), can make certain changes to their coverage once per month. Beneficiaries in these groups may use this monthly SEP to disenroll from a Medicare Advantage plan into traditional Medicare, enroll in a stand-alone Part D drug plan, or switch between Part D plans. However, they may not use the monthly SEP to enroll in Medicare Advantage or switch between Medicare Advantage plans, with the exception of individuals with full Medicaid benefits who are switching to a Fully Integrated Dually Eligible Special Needs Plan (FIDE SNP), a Highly Integrated Dually Eligible Special Needs Plan (HIDE SNP), or a coordination-only D-SNP that is an Applicable Integrated Plan (AIP) that is aligned with their Medicaid managed care enrollment. People living in nursing homes and certain other facilities may change their Medicare Advantage or Medicare Part D coverage once per month.
Medicare Advantage enrollees who wish to change plans or switch to traditional Medicare may do so between January 1 through March 31 each year, during the Medicare Advantage Open Enrollment Period. (This is in addition to the open enrollment period that runs from October 15 to December 7.) Additionally, those who have a Medicare Advantage or Medicare Part D plan with a 5-star quality rating available in their area may switch into a 5-star plan between December 8 and November 30 of the following year.
For 2026, people who select a Medicare Advantage plan based on inaccurate provider directory information in Medicare Plan Finder may qualify for a new, temporary SEP that allows them to switch to a different Medicare Advantage plan or return to traditional Medicare if they later discover that their preferred provider is not included in their plan’s network. This temporary SEP is currently limited to coverage decisions made for the 2026 plan year and runs for three months after the effective date of plan election. This is distinct from an existing SEP that allows Medicare Advantage enrollees to make changes to their coverage if their plan makes certain changes to its provider network that are deemed “significant,” such as terminating a large number of in-network providers. (See Q6 for more information about Medicare Advantage provider networks.)
The annual open enrollment period and other opportunities to switch coverage are distinct from the initial enrollment period for people who are newly enrolling in Medicare, which begins three months before a person’s 65th birthday and ends three months after it. For more information on initial enrollment, see KFF’s Medicare Open Enrollment FAQ.
Many Medicare beneficiaries have some form of additional coverage, such as a Medicare Supplemental Insurance policy (Medigap) or coverage offered by an employer or a union, that helps with Medicare’s cost-sharing requirements. Enrollment in these plans and programs is not tied to the open enrollment period, though beneficiaries may wish to take them into account when considering their options for Medicare coverage.
Medigap. People in traditional Medicare with both Part A and Part B can apply for a Medigap policy at any time of the year. Medigap policies are designed to help beneficiaries in traditional Medicare with Medicare’s deductibles and cost-sharing requirements and have standard benefits to allow for apples-to-apples comparisons across insurers. Traditional Medicare beneficiaries with a Medigap plan that covers most deductible and cost-sharing requirements may have lower out-of-pocket spending for Medicare-covered services than people with other coverage, including a Medicare Advantage plan. Medigap policies are designed to wrap around traditional Medicare, and do not work with Medicare Advantage. People enrolled in Medicare Advantage do not need (and can’t buy) a Medigap policy.
While Medigap insurers are required to issue policies to people age 65 or over, without regard to health status or diagnosed medical conditions when they first enroll in Medicare, those with pre-existing conditions may be denied a Medigap policy or face higher premiums in most states if they apply for Medigap coverage after their first six months of enrollment in Part B. People who disenroll from Medicare Advantage within 12 months of first enrolling in Medicare Advantage have a right to purchase a Medigap policy without regard to medical history, but after 12 months, they are not guaranteed Medigap coverage and may be denied a policy due to a pre-existing condition or face higher Medigap premiums if they are offered a policy.
Medigap guaranteed issue rights are different for people under age 65 who qualify for Medicare due to long-term disability. Federal law does not require Medigap insurers to sell a policy to people with Medicare under age 65, although several states do require insurers to offer at least one kind of Medigap policy to people under 65. Premiums for Medigap policies sold to people under age 65 are typically higher than policies sold to those age 65 or older. People under age 65 with disabilities who are already enrolled in Medicare will qualify for the 6-month Medigap open enrollment period when they turn 65 and become age eligible for Medicare. At this point, they can buy any Medigap policy they want without facing higher premiums or denials of coverage based on their existing medical conditions.
Employer-sponsored coverage. While employer-sponsored retiree health benefits are on the decline, more than 14.5 million people with Medicare have retiree health coverage (distinct from people with Medicare Part A only who continue to work and have health insurance through their current employer or a spouse’s current employer). Retiree health benefits may be designed to supplement either traditional Medicare or Medicare Advantage. Some employers that offer health benefits to retirees on Medicare offer these benefits exclusively through a Medicare Advantage plan. Beneficiaries with retiree health coverage offered exclusively through a Medicare Advantage plan may lose these benefits if they choose to switch to traditional Medicare during the annual open enrollment period. Similarly, employers may only offer a retiree health benefit that supplements traditional Medicare. If a person with such coverage switches from traditional Medicare to Medicare Advantage during an open enrollment period, they may lose their retiree health benefits. In fact, if a Medicare beneficiary drops their employer or union-sponsored retiree health benefits for any reason, they may not be able to get them back.
5. How Does Additional Support for Low-Income People Factor into Medicare Coverage Decisions?
Low-income Medicare beneficiaries who meet their states’ Medicaid eligibility criteria qualify for additional coverage of services through Medicaid that are not covered under Medicare, such as long-term services and supports. Additionally, Medicare beneficiaries with modest incomes may qualify for assistance with Medicare premiums and out-of-pocket costs from the Medicare Savings Programs (MSP) and Part D Low-Income Subsidy (LIS) if their income and assets are below certain amounts. Medicare beneficiaries who are eligible for Medicaid, the Medicare Savings Programs (MSPs), or Medicare Part D Low-Income Subsidies (LIS), but not yet enrolled in these programs, can enroll at any time of the year. This additional coverage and assistance may factor into how people choose to receive their Medicare benefits.
Medicaid. For people with Medicare who qualify for full Medicaid benefits, their choice of Medicare coverage can impact how they receive Medicaid benefits and the degree to which those benefits are coordinated with Medicare. In general, Medicaid wraps around Medicare coverage, with Medicare as the primary payer and Medicaid paying for costs and services not covered by Medicare. People who are eligible for both Medicare and Medicaid (dual-eligible individuals) can enroll in a Medicare Advantage plan designed for this population, such as a dual-eligible Special Needs Plan (SNP), and depending on the state and the plan, may experience a higher level of coordination of their benefits. Beginning in 2025, people who qualify for full Medicaid benefits can make certain changes to their Medicare coverage outside of the open enrollment period, up to once per month (see Q3 for further details).
Medicare Savings Programs. Through the Medicare Savings Programs (MSP), state Medicaid programs pay Medicare premiums and, in many cases, cost sharing for Medicare beneficiaries who have income and assets below certain amounts (though some states have lifted their income and/or asset thresholds above the federal limits). Specifically, states cover the Medicare Part B premium for people who qualify and may also provide assistance with Medicare deductibles and other cost-sharing requirements. People who receive MSP assistance and are enrolled in a Medicare Advantage plan may still have cost sharing associated with non-Medicare covered services offered by the plan. People who qualify for MSP but not full Medicaid benefits (sometimes referred to as “partial Medicaid benefits”) can also make certain changes to their coverage outside of the open enrollment period, up to once per month.
Part D Low-Income Subsidy. People who qualify for the Part D Low-Income Subsidy (LIS) receive varying levels of assistance toward their Part D prescription drug coverage premiums and cost sharing, depending on their income and asset levels. Dual-eligible individuals, people enrolled in the Medicare Savings Programs, and those who
ORIGINAL SOURCE:
Source link



